BALTIMORE, Maryland (Reuters) — A team at Johns Hopkins’ Department of Biology has discovered that a protein which helps neurons grow, known as ‘nerve growth factor’ (NGF), also triggers the release of insulin in the pancreas. Associate professor of biology Rejji Kuruvilla says the study may one day lead to early intervention in cases of Type 2 Diabetes.
Kuruvilla began studying NGF as a post-doctoral fellow. When setting up her laboratory at Johns Hopkins in 2005, she said her focus was on how NGF promotes the survival of nerve cells. Kuruvilla said her team of researchers took a “detour” when they found NGF receptors present in pancreatic beta-cells, which are found in clusters called islets and produce insulin.
The lab’s study, led by graduate student Jessica Houtz discovered that NGF has a second function outside the nervous system.
“I was super excited. I thought it was really cool that this unique feature of neurotrophic signaling in neurons was conserved in beta cells and had this different function outside of the nervous system,” said Houtz.
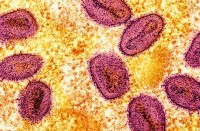
They discovered that high blood glucose causes NGF to be released from the pancreatic blood vessels, which then prompts pancreatic beta-cells to relax their skeletal barrier and release insulin.
“It’s been known for a while that glucose can re-model the skeletal barrier to secrete insulin but the downstream pathways – how glucose is sensed by the beta cells to remodel the skeletal barrier was not known. And what we found was that the NGF receptor is involved; it is the link between glucose and remodeling of the cytoskeletal barrier to secrete insulin,” said Kuruvilla.
Kuruvilla’s team tested the glucose levels in mice after genetically manipulating the function of the NGF receptor.
“What we did was to remove the NGF receptor, specifically from the pancreatic beta cells,” said Kuruvilla. The beta-cells “could make insulin but when confronted with high glucose were not able to secrete insulin in adequate amounts.”
The researchers found the same thing happens in human beta-cells, but are unsure of how the system is affected in people with diabetes.
“So it has been hypothesized or postulated that in Type 2 Diabetes that by the time a patient is diagnosed with Type 2 Diabetes, they have already lost 80 percent of beta-cell function. I think it’s absolutely critical to figure out the pathways that are important for beta cell function so that we can manipulate these pathways for early intervention of the disease, as opposed to managing a chronic disease after.”
Kuruvilla is hopeful that further studies of NGF in humans could one day lead to the development of drugs that affect the receptor activity and therefore treat pre-diabetics.
“As Rejji mentioned we’ve started to get our hands on some human islets and see how this pathway functions in human islets,” said Houtz. “But we know that the architecture and cell composition in human islets is slightly different than mouse islets so how exactly these islet micro-environment factors are functioning in human islets is still to be determined.”
Type 1 diabetes, which accounts for less than ten percent of patients, occurs when the body’s immune system destroys the cells that release insulin. Without insulin, patients’ bodies cannot absorb sugar. Most type 1 diabetics are diagnosed young.
Type 2 diabetes is often linked with obesity and can be developed at any age. In those cases patients’ bodies are unable to use insulin correctly and can suffer damage to their pancreas, although the condition can sometimes be managed through improved diet and weight loss.